Non-segmental vitiligo (NSV) is recognized as one of the more complex autoimmune skin diseases to manage in everyday clinical practice. Despite notable progress in our understanding of the immune pathways that lead to the destruction of melanocytes, treatment alternatives have traditionally been limited, especially for patients suffering from extensive or progressive forms of the disease. In a significant development aimed at expanding therapeutic options, AbbVie has submitted regulatory applications to both the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the approval of upadacitinib at a dosage of 15 mg once daily, targeting adult and adolescent patients diagnosed with NSV.
The regulatory applications are bolstered by data derived from the phase 3 Viti-Up clinical studies. “Today is a pivotal moment for patients with vitiligo and the dermatology community as we learn that upadacitinib is advancing through regulatory processes with the FDA and EMA, potentially becoming the first approved systemic treatment for adolescents and adults affected by vitiligo,” stated Christopher Bunick, MD, PhD, editor-in-chief of Dermatology Times and associate professor of dermatology at Yale School of Medicine.
“The quest for effective treatments for vitiligo has long been a substantial unmet need in the field of dermatology. The phase 3 trial data pertaining to the F-VASI and T-VASI responses at 48 weeks provide renewed hope for vitiligo patients, indicating meaningful improvements may be on the horizon.”
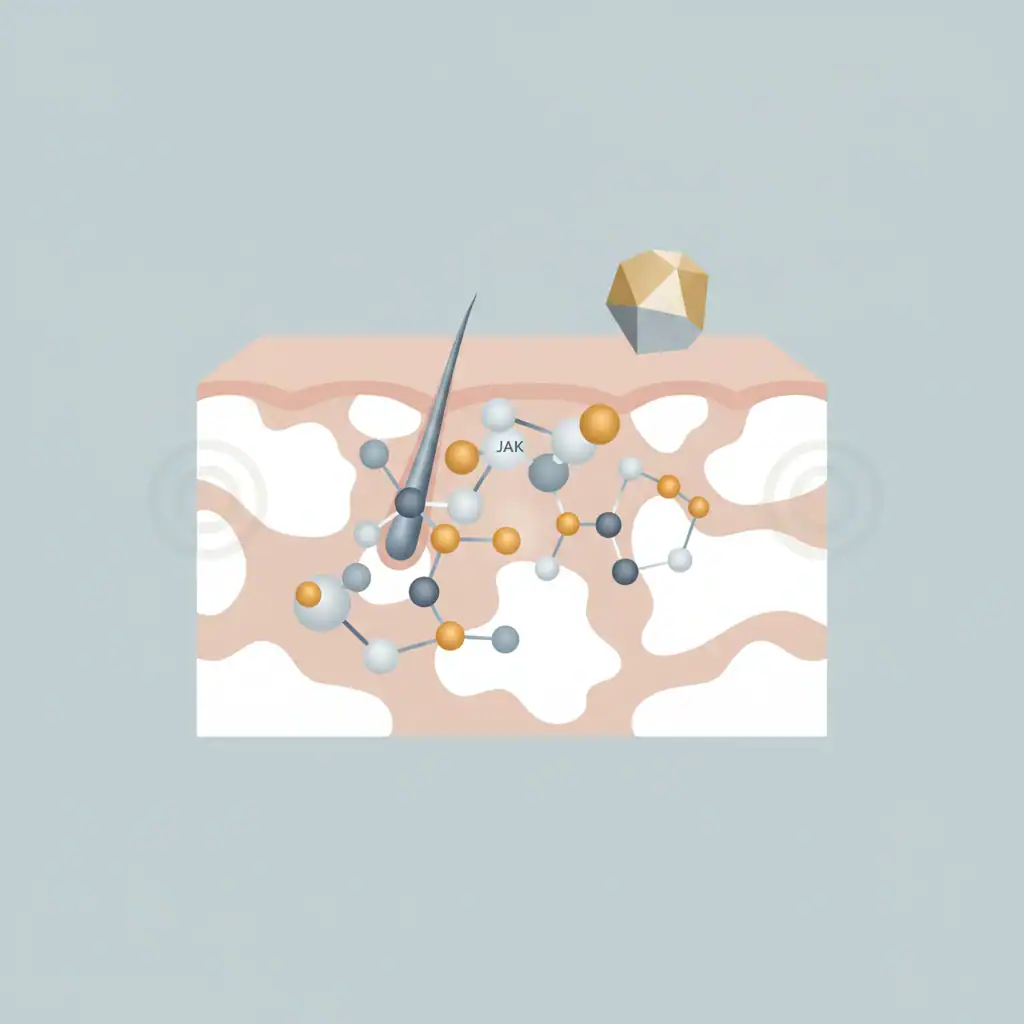
Upadacitinib adds to the expanding repertoire of anti-inflammatory therapies across various medical disciplines, showcasing the importance of optimized chemistry in driving structure-function activity and enhancing care standards for patients dealing with dermatological conditions. This treatment specifically targets JAK signaling, as well as immune pathways driven by Interferon-γ, which have been implicated in the destruction of melanocytes in vitiligo.
This mechanistic insight has sparked interest in JAK inhibitors as potentially transformative agents for modifying the disease. Upadacitinib is an oral JAK inhibitor noted for its superior inhibitory potency for JAK-1 compared to JAK-2, JAK-3, and TYK-2, based on both enzymatic and cellular assays.
Nevertheless, the clinical significance of selective JAK inhibition regarding efficacy and safety continues to be an area under active investigation. Upadacitinib already holds approvals for various immune-mediated inflammatory diseases and is being assessed for a range of dermatological and systemic autoimmune conditions, including alopecia areata and hidradenitis suppurativa.
Its exploration in the context of vitiligo is a logical progression in this developmental strategy.
The recent regulatory submissions are supported by the Viti-Up clinical studies (NCT06118411), which include two replicate phase 3 trials executed under a unified protocol.
Each trial maintained independent randomization, investigative sites, data collection, and statistical analyses, which strengthens the validity of the findings. In total, 614 participants aged 12 years and older diagnosed with NSV were enrolled across 90 sites globally.
All participants were identified as candidates for systemic therapy. During the initial phase, patients were randomized in a 2:1 ratio to receive either upadacitinib 15 mg once daily or a placebo for 48 weeks. Those who completed this period were eligible to transition into a second phase, a 112-week open-label extension where all participants received upadacitinib.
Combining the two studies allows for a comprehensive evaluation over a span of 160 weeks.
The co-primary endpoints were strategically chosen to reflect significant clinical improvement. These included the attainment of at least a 50% reduction from baseline in the Total Vitiligo Area Scoring Index (T-VASI 50) and a minimum of a 75% reduction in the Facial Vitiligo Area Scoring Index (F-VASI 75) at the 48-week mark.
Facial involvement is particularly critical due to its disproportionate impact on quality of life and patient-reported outcomes. Secondary endpoints focused on the magnitude and timing of facial re-pigmentation, including F-VASI 50 at week 48 and F-VASI 75 as early as week 24.
These metrics provide valuable insights into the speed of visible improvement and the potential for early responses with systemic therapy.
AbbVie has announced that the Viti-Up studies successfully met essential efficacy objectives, forming a strong foundation for regulatory assessment.
Nonetheless, the complete peer-reviewed publication of efficacy and safety data will be vital for clinicians to evaluate the sustainability of re-pigmentation, long-term safety, and real-world applicability. As with other JAK inhibitors, safety considerations—including the risk of infections and long-term immunologic effects—will be crucial in both regulatory and clinical decision-making.
This submission marks a significant turning point in the development of treatments for vitiligo. For clinicians, it represents the potential for systemic therapy to soon become an integral part of the therapeutic landscape for NSV, particularly for patients with widespread, progressive, or treatment-resistant disease.
Ultimately, whether upadacitinib will change standard practice will hinge on regulatory outcomes and the careful incorporation of emerging data into patient-centered care.