Acne vulgaris is a common and persistent inflammatory skin disorder, affecting approximately 50 million people worldwide each year. While current treatments can effectively manage active acne outbreaks, the challenge of addressing the resulting scarring remains significant.
Postacne scars can lead to enduring psychosocial effects, including diminished self-esteem and adverse effects on mental health. This reality highlights the urgent need for safe and effective therapeutic options, particularly for individuals with darker skin types. A variety of treatment modalities are employed to manage acne scarring, including subcision, microneedling, chemical peels, fillers, punch techniques, radiofrequency devices, and fat transfer.
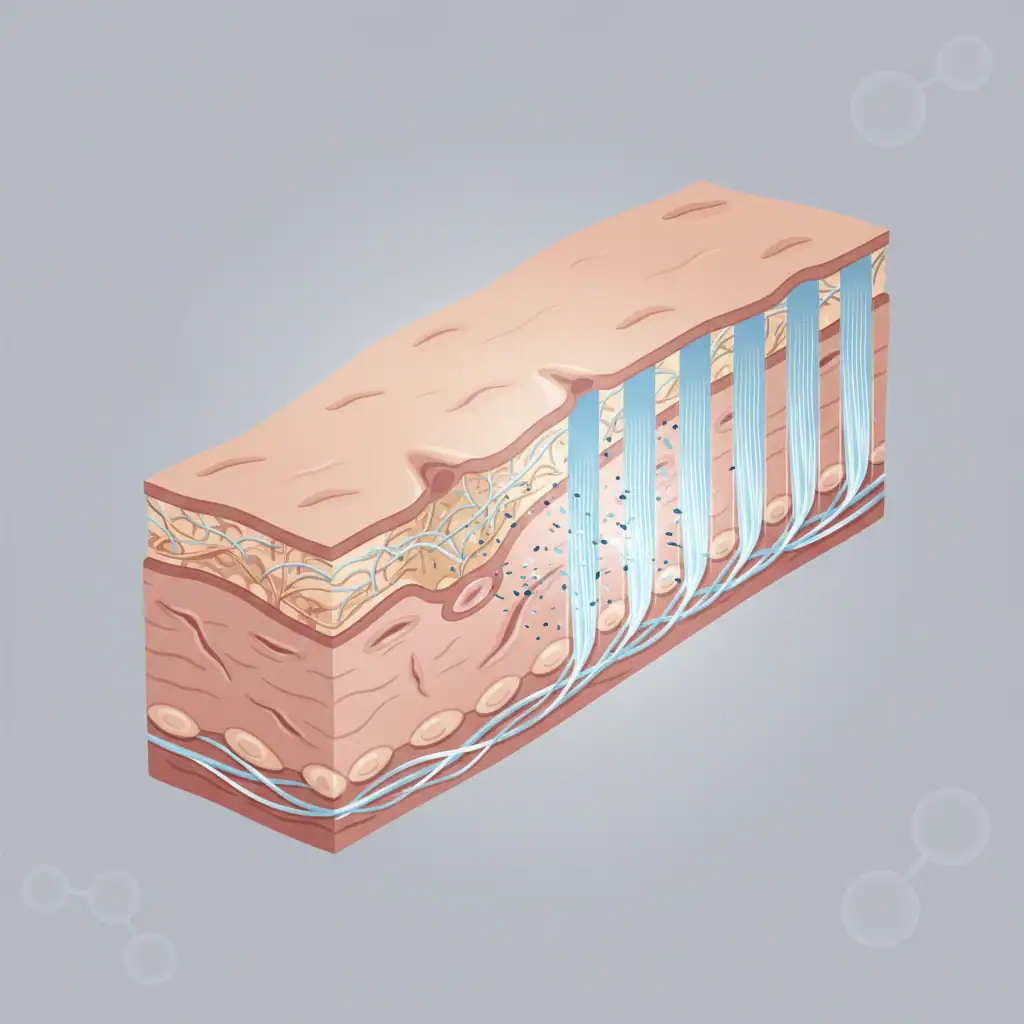
In the last two decades, laser-based resurfacing has emerged as a pivotal approach for managing scars. This technique is advantageous because it can induce controlled damage to the dermis, promote neocollagenesis, and remodel scar tissue effectively.
Among various laser treatments, fractional CO₂ laser resurfacing stands out for its effectiveness in treating atrophic acne scars. However, there are significant concerns regarding potential pigmentary complications, especially for individuals classified as Fitzpatrick skin types IV–VI, which are prevalent in Middle Eastern populations.
A recent retrospective study aimed to evaluate the efficacy and safety of a tailored dual-mode fractional CO₂ laser protocol specifically for acne scarring in Middle Eastern patients. This investigation sought to fill the gap in optimized treatment protocols for darker skin tones by integrating targeted high-fluence treatments for individual scars with lower-fluence resurfacing for the surrounding skin.
This retrospective chart review examined 57 adults treated between 2015 and 2018. All participants were at least 18 years old and had Fitzpatrick skin types IV or V, presenting with clinically evident postacne scarring. Exclusion criteria included individuals with active inflammatory skin conditions, recent cosmetic interventions, those using isotretinoin, pregnant women, or individuals with systemic illnesses affecting wound healing.
Each patient underwent four sessions of fractional CO₂ laser treatment utilizing the eCO₂ system (Lutronic), with sessions spaced 6 to 8 weeks apart. The treatment involved a dual-mode approach:
Post-treatment care included the application of topical antibiotic ointment, strict measures for photoprotection, avoiding mechanical trauma during the healing phase, and antiviral prophylaxis when necessary.
Follow-up photography was conducted three months after the final treatment session to evaluate outcomes. Treatment response was assessed through both subjective and objective measures. Subjective evaluations utilized the Goodman and Baron Global Acne Scarring Grading System (GASS), performed by a blinded dermatologist.
For objective assessment, the VISIA complexion analysis system was employed to quantify changes in skin texture and spot characteristics through percentile, score, and count metrics.
The study found that GASS scores significantly improved following treatment, decreasing from a mean of 10.12 at baseline to 8.04 post-treatment. Improvements were most notable in patients with moderate atrophic scars, while those with mild macular scars exhibited nonsignificant changes. Interestingly, patients presenting with higher baseline severity experienced more substantial improvements, aligning with existing literature on laser resurfacing.
Analysis with the VISIA system indicated a statistically significant enhancement in spot percentile scores, although other individual texture and spot parameters did not reach significance. Nevertheless, regression modeling demonstrated that VISIA metrics accounted for over one-third of the variance in GASS scores, affirming their utility as a supplementary assessment tool rather than a standalone measure.
Crucially, no clinically significant post-inflammatory hyperpigmentation was recorded, suggesting that the customized fluence and density strategy effectively mitigates pigmentary risks in darker skin types.
This study highlights the effectiveness of fractional CO₂ laser resurfacing as a viable treatment for atrophic acne scars in Middle Eastern patients when specific treatment parameters are meticulously tailored. The dual-mode approach—merging high-fluence focal treatment with lower-fluence field resurfacing—appears to optimize both efficacy and safety, particularly for skin types at a heightened risk for dyschromia.
As consistent with prior findings, boxcar and rolling scars demonstrated better responses compared to ice-pick scars, which may necessitate additional techniques for optimal results.
As a retrospective analysis lacking a control group, these findings should be interpreted with caution. The sample size was limited, follow-up durations were relatively brief, and acute adverse effects could not be systematically monitored. However, the integration of validated subjective grading with objective imaging bolsters the study’s conclusions.
Overall, this research offers clinically significant evidence supporting tailored fractional CO₂ laser protocols for treating acne scarring in individuals with darker skin phototypes. While subjective grading systems remain the most sensitive indicators of clinical improvement, objective tools like VISIA may provide important supplementary insights.
Future research should include larger prospective, controlled trials to refine treatment protocols and validate long-term outcomes.