This week, Sagimet Biosciences shared encouraging results from the 52-week data of its license partner Ascletis Pharma regarding an open-label phase 3 clinical trial. This trial evaluated the long-term safety of denifanstat (ASC40) tablets in individuals suffering from moderate to severe acne vulgaris. The findings contribute significant insights into the safety profile and sustained efficacy of this groundbreaking, once-daily oral fatty acid synthase (FASN) inhibitor, which introduces a novel mechanism for treating acne.
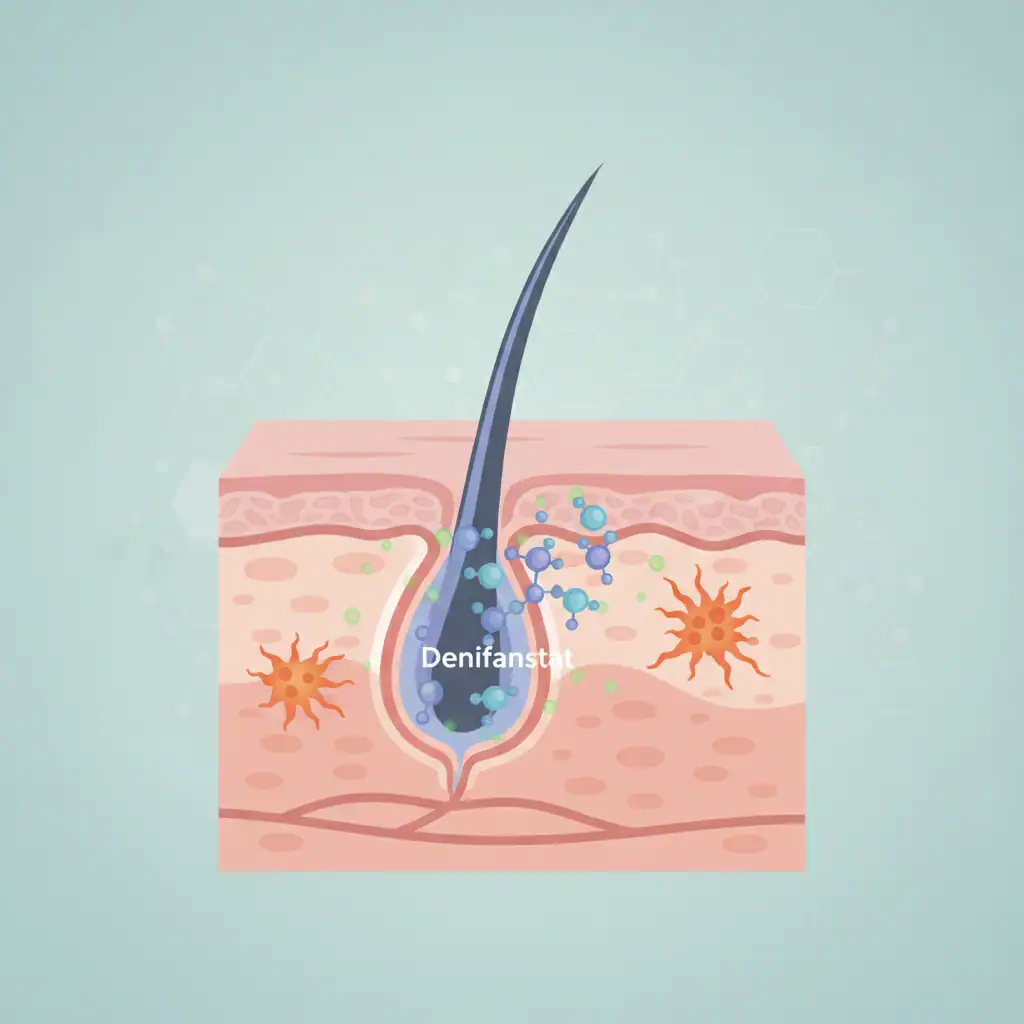
Denifanstat is a small-molecule FASN inhibitor specifically designed to target de novo lipogenesis, a metabolic pathway linked to the production of lipids in the sebaceous glands and the development of acne. Ascletis is spearheading the clinical development of this agent as ASC40 for acne treatment in China, while Sagimet is advancing denifanstat on a global scale for metabolic dysfunction–associated steatohepatitis.
Sagimet has previously granted Ascletis an exclusive license to develop and market denifanstat for acne within China. The results recently released stem from the ASC40-304 trial (NCT06248008), a multicenter, open-label phase 3 extension study primarily aimed at evaluating long-term safety.
The trial involved 240 patients diagnosed with moderate to severe acne who had previously completed a 12-week randomized, double-blind, placebo-controlled phase 3 study (ASC40-303; NCT06192264). These findings were presented at the 2025 European Academy of Dermatology and Venereology Congress held in Paris, France. Dr. Neal Bhatia, the medical director of Therapeutics Clinical Research in San Diego and a former vice president of the American Academy of Dermatology, commented on the data: “Following the 12-week data from the phase 3 randomized double-blind denifanstat trial in patients with moderate to severe acne, results from the 40-week open-label study are even more encouraging.”
He further noted, “For patients with moderate to severe acne, who are often underserved by existing treatments, the advent of a new therapeutic option would be a significant enhancement to the current treatment arsenal.” In this extension study, all participants were administered oral denifanstat at a daily dose of 50 mg for up to an additional 40 weeks.
Patients who had initially been randomized to receive denifanstat in the parent study thus accrued up to 52 weeks of cumulative drug exposure. The primary endpoints of ASC40-304 focused on safety and tolerability throughout the extended treatment duration, while secondary endpoints assessed the persistence of efficacy.
Overall, denifanstat was reported to be generally well-tolerated among trial participants. The scope of treatment-emergent adverse events was limited, with only two categories of events occurring in 5% or more of the treated subjects: dry eye syndrome (5.5%) and dry skin (5.2%).
These adverse events align with the anticipated effects on sebaceous and related lipid pathways and were not associated with significant morbidity. All adverse events related to denifanstat were characterized as mild to moderate in severity.
No incidents of treatment-related Grade 3 or 4 adverse events were reported, and there were no permanent discontinuations linked to adverse events. Although hair thinning is a potential concern with treatments that alter lipid metabolism, only one patient experienced this as a Grade 1 event, which resolved within 8 weeks without any dose adjustments.
Serious adverse events were infrequent and not attributed to denifanstat.
While the extension study was not primarily designed to assess efficacy, participants exhibited improvements across various clinical endpoints beyond those recorded at week 12 in the double-blind trial.
Secondary efficacy measures included:
Patients demonstrated continued progress across these measures with long-term therapy, indicating a durable or incremental benefit from ongoing FASN inhibition. Detailed efficacy data is anticipated to be presented at forthcoming scientific congresses and published in peer-reviewed journals.
Dr. Bhatia commented on the current landscape of acne treatments: “Unfortunately, the pipeline for acne therapies is drying up, and overall, acne has been an underdeveloped disease market for the past four decades. Dermatologists have been striving to reduce reliance on oral antibiotics for managing moderate to severe acne over the last ten years, and denifanstat appears to offer a promising alternative to the over 5 million prescriptions written by dermatologists annually. Although the mechanisms differ, having another treatment option is very welcome.”